Rheumatic fever is a delayed autoimmune reaction in genetically predisposed individuals to group A, β-hemolytic, streptococcal pharyngitis. It is a self-limited disease that may involve joints, skin, brain, serous surfaces, and the heart. If no cardiac valve damage, then the disease would be of little practical consequence
- Ages 5-15 yrs are most susceptible
- Rare <3 yrs
- Girls>boys
- Common in 3rd world countries
- Environmental factors-- over crowding, poor sanitation, poverty,
- Incidence more during fall ,winter & early spring
- Delayed immune response to infection with group.A beta hemolytic streptococci.
- After a latent period of 1-3 weeks, antibody induced immunological damage occur to heart valves,joints, subcutaneous tissue & basal ganglia of brain
- Step I - primary prevention (eradication of streptococci)
- Step II - anti inflammatory treatment (aspirin,steroids)
- Step III - supportive management & management of complications
- Step IV - secondary prevention (prevention of recurrent attacks)
Kawasaki Disease
Kawasaki disease is an acute self-limited vasculitis of childhood that is characterized by fever, bilateral nonexudative conjunctivitis, erythema of the lips and oral mucosa, changes in the extremities, rash, and cervical lymphadenopathy.
Coronary artery aneurysms or ectasia develop in 15% to 25% of untreated children and may lead to ischemic heart disease or sudden death
- First described in Japan in l967 by Tomisaku Kawasaki
- Known to occur in both endemic and community-wide epidemic forms in the Americas, Europe, and Asia in children of all races.
- Leading cause of acquired heart disease in children in the U.S.
- Children with KD below 15 years -January 1994 to December 2008.
- 196 children were diagnosed as KD. Of these, 80 from Chandigarh.
- Comparison of yearly data revealed increasing incidence from 0.51 cases in 1994 to 4.54 cases per 100,000 children below 15 years of age in 2007.
- Monthly distribution of disease showed two peaks with a maximum number of cases presenting in October followed by a second peak in May with a nadir in the month of February.
- Increasing incidence of KD in Chandigarh could be due to increasing clinical recognition as a result of greater awareness among pediatricians.
Criteria for Kawasaki disease (KD)
Diagnosis of KD follows the criteria outlined in the fifth edition of the diagnosis guidelines for KD,2 which requires that at least five of the following six principal symptoms are present :
- fever persisting ≥5 days (including fever that subsides before the fifth day in response to therapy);
- bilateral conjunctival congestion;
- changes in lips and oral cavity: reddening of lips, strawberry tongue, diffuse injection of oral and pharyngeal mucosa;
- polymorphous exanthema;
- changes in peripheral extremities:reddening of palms and soles, indurative edema (initial stage);membranous desquamation from fingertips (convalescent stage);
- acute non-purulent cervical lymphadenopathy.
Stage 1 (0 – 9) days
- Microvascular angitis
- Acute endarteritis and perivasculitis of major coronaries
- Pericarditis, myocarditis, endocarditis
- Cause of death : Heart failure & dysrhythmia
Stage 2 (12-25 days)
- Panvasculitis of major coronary arteries with aneurysm & thrombus formation
- Intimal proliferation of coronary arteries
- Pericarditis, Myocarditis,Endocarditis
- Causes of death – same as stage 1,MI, Aneurysmal rupture
Stage 3 (28 – 31 days)
- Granulation of coronary arteries,
- Marked intimal thickening
- Disappearance of microvascular angitis
- Cause of death : MI
Stage 4 (40 days – 4 years)
- Scarring, stenosis, calcification, recanalisation of coronary arteries
Positive echocardiography
- z score of LAD or RCA 2.5
- Coronary arteries meet Japanese Ministry of Health criteria for aneurysms
- Other suggestive features exist, including perivascular brightness, lack of tapering, decreased LV function, mitral regurgitation, pericardial effusion, or z scores in LAD or RCA of 2–2.5.
Japan Kawasaki disease research committee
Coronary artery is abnormal if
- The internal diameter is > 3mm in children <5 years ofage
- >4 mm in children >5 years of age
- The internal diameter of a segment (measured from inner edge to inner edge excluding points of branching) measures 1.5 times that of an adjacent segment
- coronary artery lumen is clearly irregular
Not based on an individual patient’s body size.
Coronary aneuryms
- Major sequelae related to coronary arterial involvement
- Initial echocardiogram done as soon as the diagnosis is suspected
- Establishes a baseline for longitudinal follow-up of coronary artery morphology, LV and left valvular function and the evolution and resolution of pericardial effusion
Risk scores for predicting aneurysms
Four of the following criteria, assessed within 9 days of onset of illness
- White blood cell count >12000/mm3
- Platelet count <350000/mm3
- CRP >3+
- Hematocrit <35%
- Albumin <3.5g/dL
- Age £ 12 months;
- Male sex
Common sites (from highest to lowest frequency)
- Proximal LAD and proximal RCA
- LMCA
- LCX
- Distal RCA
- Junction between the RCA and posterior descending coronary artery
- Z scores are available for only the LMCA, proximal LAD and proximal RCA
- LMCA involvement does not involve the orifice
- Rarely occurs without associated ectasia of the LAD, LCX, or both arteries
- Lack of normal tapering and perivascular echogenicity or “brightness” of coronary arteries
- Saccular - axial and lateral diameters nearly equal
- Fusiform - symmetric dilatation with gradual proximal and distal tapering
- Ectatic if coronary artery larger than normal (dilated)
- Aneurysms as per size
- Small (<5mm internal diameter)
- Medium (5 – 8mm internal diameter)
- Giant (>8mm internal diameter)
Spontaneous regression of aneurysms
- Approximately 50% show angiographic regression of aneurysms
- Usually occurs by myointimal proliferation, rarely by organisation and recanalisation of a thrombus
- 0, 2 weeks, 6 – 8 weeks for uncomplicated cases
- More frequent for children at higher risk (e.g., those who are persistently febrile or who exhibit coronary abnormalities, ventricular dysfunction, pericardial effusion or valvular regurgitation)
- Follow up echocardiography - 1 year after the onset of the illness
- Myocarditis
- Depressed ventricular contractility
- Assessment of LV function
- Evaluating regional wall motion
- Aortic root for mild aortic root dilation
- Pericardial effusion
- Angiography, IVUS, TEE
- MRI and MRA - delineate coronary artery aneurysms and provide data regarding flow profile
- 64 slice CT scan
- Cardiac stress testing for reversible ischemia
- Types of stress tests reported in children include nuclear perfusion scans with exercise, exercise echocardiography and stress echocardiography
- MRI stress imaging with quantification of regional perfusion
- Myocardial contrast echocardiography - to assess myocardial perfusion
- Stress test - guide for invasive evaluation as well as for catheter or surgical intervention
- Choice of stress modality should be guided by institutional expertise as well as by the age of the child
Cardiac catheterisation and angiography
- Coronary angiography
- More detailed definition of coronary artery anatomy
- Detect coronary artery stenosis or thrombotic occlusion
- Determine the extent of collateral artery formation
- Potential benefits of the procedure to be compared with risks and cost
- Recommended 6 – 12 months after the onset of illness or sooner if indicated clinically
- Not recommended in pts with mild ectasia or small fusiform aneurysms
- Sudden death from MI may occur many years later in individuals who as children had coronary artery aneurysms and stenoses.
- Many cases of fatal and nonfatal MI in young adults have been attributed to “missed” Kawasaki disease in childhood
Onset : 40% within 3 months
73% within first yr.
20% occur more than 2 yrs out
5% greater than 6 yrs
Symptoms : 63% had symptomatic MI
54% presented in shock
chest pain : <4yr 20%,
>4yr 80%
- Activity : Only 14% had MI during play or exercise. 63% during sleep or at rest.
- Mortality : 22% died during the first MI
Infants<1yr, 43% died
- Prognosis: 41% asymptomatic. Cardiac symptoms due to MR, decreased LV EF, LV aneurysm,angina. 16% of survivors had second MI, 63% died.
- Reduction of inflammation within the coronary artery & myocardium
- Prevention of thrombosis by inhibiting platelet aggregation
Initial treatment
Aspirin
- Does not lower the frequency of coronary abnormalities
- 80 – 100mg/kg/day in 4 doses until 48 to 72 hours after fever cessation
- Continue as low-dose aspirin (3-5mg/kg/day) and maintain until the patient shows no evidence of coronary changes by 6 – 8 weeks after the onset of illness
- If coronary abnormalities, aspirin may be continued indefinitely
- Concomitant use of ibuprofen should be avoided
Aspirin and Influenza vaccine
- Reye syndrome is a risk & has been reported in patients taking high dose aspirin for a prolonged period after kawasaki disease.
- Low dose aspirin for antiplatelet effect - less risk
- Children who are taking salicylates longterm should receive annual influenza vaccine
Intravenous immunoglobulin (IgG)
- Reduces the prevalence of coronary artery abnormalities
- Generalized anti-inflammatory effect
- 2g/kg as single infusion within first 10 days of illness and, if possible, within 7 days of illness
- Given to children presenting after the 10th day of illness if persistent fever or aneurysms and ongoing systemic inflammation (elevated ESR or CRP)
- IVIG ,5% of children develop at the least transient coronary artery dilation and 1% develop giant aneurysms
Steroids
- High dose intravenous methyl prednisolone
- Greater rate of improvement in coronary abnormalities
- No significant difference in the prevalence of coronary aneurysms
- At present, usefulness not well established
- Multicenter randomized, placebo-blind trial in progress
Treatment of patients who failed to respond to initial therapy
- IVIG
- Retreatment with IVIG, 2g/kg if persistent or recrudescent fever ³ 36 hours after completion of the initial IVIG infusion
- Steroids
- Effects on coronary artery abnormalities still uncertain
- To be restricted to cases in which ³2 infusions of IVIG have been ineffective
- Most commonly used – intravenous pulse methylprednisolone, 30mg/kg for 2 – 3 hours, administered once daily for 1 – 3 days
Representative scoring systems for evaluating potential IVIG resistance
Kobayashi score8 (≥5 points; 76% sensitivity, 80% specificity) Cut off points
Sodium ≤133 mmol/L
2 Day of illness at initial IVIG
Day 4 or earlier 2 (= KD diagnosed) AST ≥100 IU/L 2
Neutrophil ratio ≥80% 2 CRP ≥10 mg/dL 1
Platelet counts ≤30.0 × 104/mm3 1
Age ≤12 months 1
Egami score9 (≥3 points; 78% sensitivity, 76% specificity)
ALT ≥80 IU/L 2
Day of illness at initial IVIG Day 4 or earlier 1 (= KD diagnosed) CRP ≥8 mg/dL 1
Platelet counts ≤30.0 × 104/mm3 1
Age ≤6 months 1
Sano score10 (≥2 points; 77% sensitivity, 86% specificity)
AST ≥200 IU/L 1
Total bilirubin ≥0.9 mg/dL 1
CRP ≥7 mg/dL 1
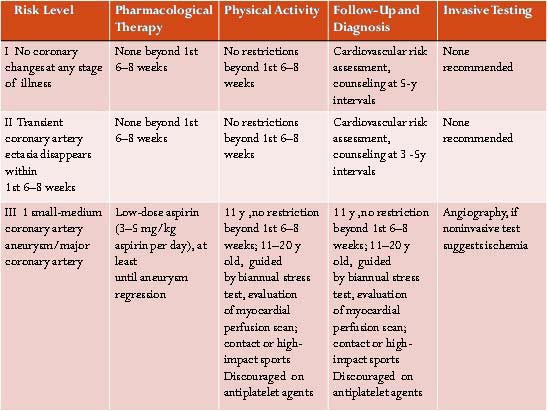
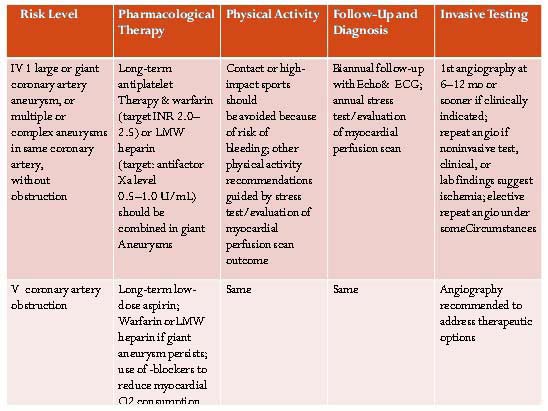
Prevention of Thrombosis in patients with Coronary Disease
- Low-dose aspirin for asymptomatic patients with mild and stable disease
- Aspirin with or without dipyridamole or clopidogrel
- Anticoagulant therapy with warfarin or low-molecular-weight heparin
- anticoagulant and antiplatelet therapy (warfarin/Heparin plus aspirin)
Antithrombotic regimen for patients with giant aneurysms
- Low-dose aspirin together with warfarin, maintaining an INR of 2.0 to 2.5
Treatment of Acute Myocardial Infarction
- Streptokinase, urokinase and tissue plasminogen activator (tPA) has been administered with varying success rates.
- Both Intracoronary and intravenous thrombolysis tried
- No randomized, controlled trials in children
- Reduced dose thrombolytic therapy + glycoprotein IIb/IIIa inhibitor - lower rates of reocclusion and reinfarction
- Immediate coronary angioplasty or stent placement used in a small number of children
- Should be based on that which can be administered with the greatest expertise in a timely fashion
Surgical treatment
- Indications
- Reversible ischemia on stress-imaging
- Viable myocardium
- No appreciable lesions present in the artery distal to the planned graft site
- One panel of experts considered the following as indications for surgery
- Severe occlusion of the main trunk of the LMCA
- Severe occlusion of >1 major coronary artery
- Severe occlusion in the proximal segment of the LAD
- Collateral coronary arteries in jeopardy or
- All the above
- Surgery preferred in pts with severe LV dysfunction
Cardiomyopathy
Cardiomyopathy is a somewhat loose term used for group of diseases of the heart muscle that is not secondary to hypertension, valvular or, congenital heart disease or pulmonary vascular disease
Cardiomyopathy is typically divided into several subtypes :
- hypertrophic cardiomyopathy,
- glycogen cardiomyopathy,
- dilated cardiomyopathy,
- restrictive cardiomyopathy, and
- arrhythmogenic right ventricular cardiomyopathy.
Correctable causes of DCM in children
- ALCAPA
- COA/ CRITICAL AS
- TAKAYASU ARTERITIS
- TACHYCARDIOMYOPATHY- EAT,PJRT,C/C ATRIAL FLUTTER
- HYPOCALCEMIA [ IN NEWBORNS]
- INFANTILE BERI BERI
- CARNITINE DEFICIENCY
- HYPOPHOSPHATEMIA
- SELENIUM DEFICIENCY
- CONGENITAL MR
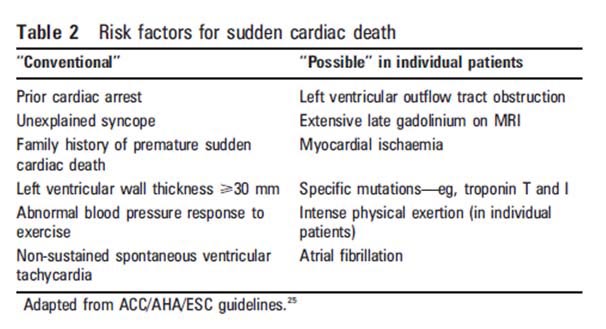
Hypertrophic cardiomyopathy (HCM)
Hypertrophic cardiomyopathy (HCM) is a treatable disease compatible with a normal lifespan.
| Risk Factor |
Imaging modality |
| Maximum wall thickness ≥ 3 cm |
Echocardiography, CMR, Cardiac CT |
| End-stage HCM ( EF < 50%) |
Echocardiography, radionuclide angiography, CMR, cardiac CT |
| Apical aneurysms |
Contrast echocardiography, CMR, and Cardiac CT |
| LVOT gradient ≥ 30 mm Hg |
Doppler echocardiography |
| Perfusion defects |
SPECT (though no association in some studies) |
| Reduced coronary flow reserve |
PET (observations limited to very few patients) |
| LGE (presence and extent) |
CMR (evidence not conclusive) |
It is the most common inherited cardiac disease with an incidence of 1in 500
- More than 1400 mutations account for approximately 50% of identifiable patients with HCM.
- The most common cause of sudden cardiac death among young adults
Hypertrophic cardiomyopathy (HCM) is a relatively common disorder with a prevalence of about 1:500.
It is recognized clinically by the presence of cardiac hypertrophy in the absence of an increased external load. Echocardiographically, it is associated with preserved systolic, but impaired diastolic, function. Hypertrophy is asymmetric in about two thirds of cases, with the septum being the predominant site of involvement. Significant left ventricular outflow tract obstruction is observed in approximately one-quarter of cases.
HCM is usually inherited as an autosomal dominant trait. The first gene linked to HCM was reported in 1990. This was the gene encoding cardiac b-myosin heavy chain (MYH7), a component of the sarcomere, the contractile unit within the cardiomyocyte. The sarcomere is an immense protein complex that is organized into thick and thin filaments that, in the presence of calcium and ATP, slide past each other, thereby generating contractile force.After the discovery of mutations in MYH7, mutations in another 10 sarcomeric genes were linked to HCM, leading to the proposition that HCM was a disease of the sarcomere. Most commonly affected are the MYH7 and the MYBPC3 genes, with the other genes accounting for far fewer cases. Mutations in sarcomeric genes account for about 60% of cases of HCM.
Dilated cardiomyopathy (DCM)
Dilated cardiomyopathy (DCM) is characterized by left ventricular chamber enlargement and systolic dysfunction, with normal or a modest increase in ventricular wall thickness. It has an estimated prevalence of 1 : 2500. Affected individuals gradually develop heart failure, often in association with lifethreatening atrial or ventricular arrhythmias. The disease is familial in about 35% of cases, pointing to an important role of genetics in disease pathogenesis [10]. In such cases, inheritance is most commonly autosomal dominant, but autosomal recessive, X-linked, or matrilinear (mitochondrial) inheritances also occur. DCM has been linked to 25 different chromosomal loci and genes. Known mutations affect proteins with a wide range of unrelated functions. Mutations have been identified in several components of the myocyte cytoskeleton, which, through a complex network of proteins, links the sarcomere to the sarcolemma and extracellular matrix and functions to transmit force generated during contraction. Cytoskeletal components found to be associated with DCM include cardiac muscle LIM protein (MLP), cypher/ZASP (LBD3), d-sarcoglycan (SGCD), desmoplakin (DSP), desmin (DES), dystrophin (DMD), telethonin (TCAP), and vinculin (VCL). A myriad of phenotypes, besides DCM, are associated with lamin A/C mutation, including Emery–Dreifuss muscular dystrophy type B1 and Charcot–Marie–Tooth disease. Several genes encoding sarcomeric proteins linked to HCM, including TTN, ACTC, TPM1, MYH7 and TNNT2, may also cause DCM. Other genes linked to DCM include genes encoding ion channel subunits. One of these is SCN5A, which encodes the pore-forming subunit of the cardiac sodium channel. Conduction disease and atrial fibrillation are a common finding in patients with DCM harbouring mutations in SCN5A. Another ion channel gene subunit linked to DCM is the sulfonylurea receptor 2A (SUR2A), which is the regulatory subunit of KATP channels in the heart. DCM is also caused by mutation in phospholamban (PLN), which has an essential role in calcium metabolism by modulating calcium
- Viral Myocarditis clinically overlaps with DCM.
- Symptoms and functional consequences are related to the severity of ventricular dysfunction.
- Clinical diagnosis of myocarditis is based on short history, clinical features of cardiac failure and echo evidence of ventricular dysfunction.
- Histologic evidence of inflammation on biopsy/necropsy.
- Viral serology may be helpful in some cases
Differentiation between these two has major impact on management and prognosis- Viral myocarditis needs aggressive management
Etiology
- Acute and chronic viral myocarditis- coxsackievirus, adenovirus, HIV
- Hereditary Cardiomyopathies- autosomal dominant, autosomal recessive, X-linked, mitochondrial
- Drugs-Antimitotic (Adriamycin, Doxorubicin), sympathomimetics,
- End-stage hypertrophic cardiomyopathy
- Endocrine- GH deficiency, hyper/hypothyroidism, hypocalcemia, Dibete Mellitus , pheochromocytoma
- Inborn errors of metabolism-
- Collagen vascular disease
- Muscular dystrophies
- Nutritional deficiency- selenium, carnitine, thiamine
- Toxins- cobalt, lead
- The variety of causes that can eventually result in DCM suggest that the disorder is the final common pathway for a number of mechanisms that produce myocardial damage, including cytotoxic, metabolic, immunologic, and infectious mechanisms
Familial DCM
- In 9% to 20% of cases of DCM, asymptomatic relatives have left ventricular dilatation. This serves as a marker for later progression to DCM
- Familial DCM most commonly inherited as autosomal dominant trait, conferring 50% risk
- Less commonly X-linked asymptomatic males have been reported
- Autosomal Recessive and maternally inherited forms are rare and they are usually associated with neuromuscular disease or metabolic disease.
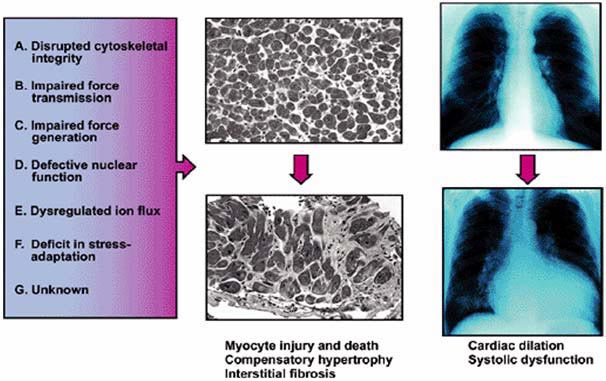
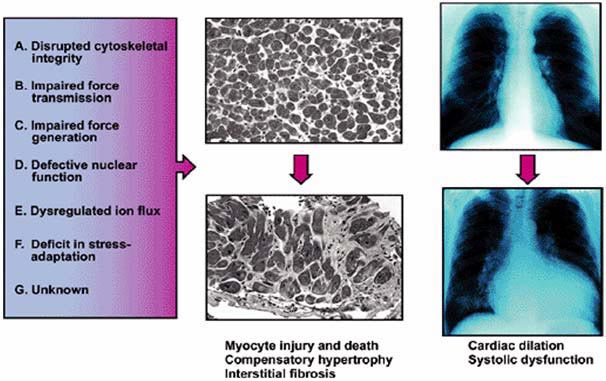
Pathogenesis---Pathology---Clinical
Clinical Features
- Older Child :
– Exercise intolerance
– Dyspnea on exertion
– Tacycardia
– Palpitations
– Chest pain
– Syncope or near syncope
– Occasionally cardiovascular collapse/sudden death
- Infants
- Respiratory distress
- Preceding history viral respiratory or GIT infection
- Abdominal distension
- Poor feeding
- Subacute presentation as failure to thrive
- Short History suggests viral myocarditis
Investigations
- Biochemical Investigations :
- Complete Hemogram including ESR
- Electrolytes, Calcium, Magnesium
- C- Reactive Protein
- ECG
- X- Ray Chest
- ECHO
- MRI- Gives accurate estimation of LV/RV volumes, masses, and ejection fraction.
- Cath- primarily performed for endocardial biopsy
- Rarely hemodynamic assessment if there discrepancy in findings on echo
- Important if cardiac transplantation is considered to measure PA pressures and vascular resistance
Management
- The aim must be to offer definitive treatment at the earliest.
- All correctable causes with CHF require surgery/intervention at the earliest.
- Conditions like tachy-cardiomyopathy and ALCAPA easily mistaken for dilated cardiomyopathy.
Medical treatment is for a few days/weeks when you are planning surgery or for those few conditions not amenable to surgery
Acute Phase
- Acutely Sick patient in cardiac failure
- Intubation may be required
- Inotropes- Dopamine, Dobutamine
- IV diuretics
- Role of IVIg
- May reduce progression to DCM if given within 14 days of onset in viral myocarditis
- 2gm/kg i.v. single dose
ACE inhibitors
- ACE inhibitors lower aortic pressure and SVR, do not affect PVR significantly, and lower LA and RA pressures in pediatric patients with heart failure.
- In infants with shunt lesions and pulmonary hypertension, ACE inhibitors decrease left-to-right shunt in those infants with elevated SVR.
- ACE inhibitors induce a small increase in LVEF, LV fractional shortening, and systemic blood flow in children with LV dysfunction, MR and AR.
Some studies have demonstrated survival benefit in patients with severe LV dysfunction from DCM in pediatric patients
- Hypotension and renal failure, if they occur, usually occur within 5 days. In most cases, recovery is seen after reduction or cessation of the drug.
- Smaller doses are administered initially to prevent excessive hypotension, and doses are increased gradually to the target dose.
- Captopril is administered orally, usually every 8 hours in a dose of 0.3 to 1.5 mg/kg/day in children.
- Enalapril is administered orally, once or twice a day (0.1 to 0.5 mg/kg).
Carvedilol
- Prevents and reverses adrenergically mediated intrinsic myocardial dysfunction and remodeling.
- Other beneficial effects include decreased stimulation of other neurohormonal systems, anti-arrhythmic effects, coronary vasodilation, negative chronotropic effects, and antioxidant effects.
- Useful adjunct to standard therapy for heart failure.
- Many studies (small number) showed significant improvement in symptoms, positive effects on ventricular remodeling and significant reductions in end-diastolic and end-systolic diameters, with an increase in LVEF. Increased survival and reduced need for transplantation in some studies.
- The results of a multicenter, randomized, double-blind, placebo-controlled study of 161 children and adolescents with symptomatic systolic heart failure from 26 US centers (Shaddy et al 2006) suggested that carvedilol did not significantly improve clinical heart failure outcomes. The finding was largely due to unexpected (55%) improvement in Placebo arm.
- Treatment is initiated with a dose of 0.01 mg/kg/day and titrated to 0.2 mg/kg/day.
- Frequent dose adjustments may be necessary and although side effects are common they are well tolerated.
Follow Up
- Regular out patient f/u with hospitalisation for episodic worsening.
- Attention to feeding, weight gain, side effects of drugs
Prognosis In DCM
- DCM in children may recover completely in as many as 50%.
- Patients whose EF has improved over the first 1 to 6 months have better prognosis.
- Young age at presentation has been considered with better outcome by some groups.
- Familial CM and persistent CHF have poor prognosis.
- Marked elevation of LVEDP, presence of ventricular arrhythmias, tissue diagnosis of Endocardial fibroelastosis have poor outcome
- Tissue biopsy diagnosis of myocarditis has been shown with better prognosis.
- Coexistence of RV dysfunction is associated with poor outcome
Restrictive Cardiomyopathy
Restrictive cardiomyopathy is a rare disorder characterized by a normal or decreased volume of both ventricles, associated with bi-atrial enlargement, impaired ventricular filling with restrictive physiology, normal myocardial wall thickness, and normal or near-normal systolic function. A mutation has been described in cardiac troponin I (TNNTI3) in a family in which carriers exhibited restrictive or hypertrophic cardiomyopathy. Additional TNNTI3 mutations were also found in unrelated patients with restrictive cardiomyopathy
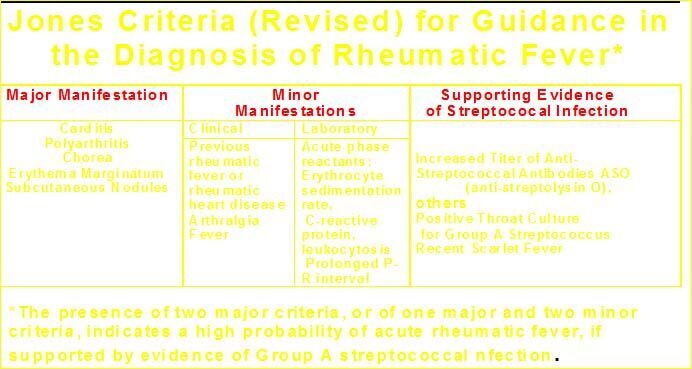
DIAGNOSIS OF RHEUMATIC FEVER
Clinical and laboratory Criteria
Major criteria (more specific)
– Carditis
– Polyarthritis
– Chorea
– Subcutaneous nodule
– Erythema marginatuma
Minor criteria (less specific)
– Fever
– Polyarthralgia
– ESR, CRP, polymorphonuclear leukocytosis (follow standard laboratory values)
– *ECG: Prolonged PR interval
Supportive evidence of preceding streptococcal infection (essential except for diagnosis of Chorea)
Anti streptolysin O ASO titer :
>333 unit for children and > 250 for adults.
Anti-deoxyribonuclease B (normal values Anti DNase B titer 1:60 unit in preschool, 1:480 units in school children & 1:340 in adults)
History of (within previous 45 days)
– streptococcal sore throat
– scarlet fever
– positive throat culture
– positive rapid streptococcal antigen detection test
* Normal upper range; – PR Interval:3-12 yrs:0.16sec; 12-14 y: 0.18 sec; >17y:0.20 sec)
First episode : Two major or one major and two minor criteria plus supportive evidence of previous streptococcal throat infection
Recurrence in a patient without established heart disease :
Two major or one major and two minor criteria + supportive evidence of previous streptococcal throat infection.
Recurrence in a patient with established heart disease :
Two minor criteria and supportive evidence of previous streptococcal throat infection.
Rheumatic chorea and insidious onset rheumatic carditis :
No requirement of other major manifestations or supportive evidence of streptococcal sore throat infection
Indicators of recurrence of rheumatic fever in established heart disease :
- new murmur / change in pre-existing murmur;
- pericardial rub (and other evidence of pericarditis); and
- unexplained congestive heart failure (CHF), including cardiomegaly.
Terminology
Recurrence : A new episode of rheumatic fever following another GABHS infection; occurring after 8 week following stopping treatment.
Rebound : Manifestations of rheumatic fever occurring within 4-6 wk of stopping treatment or while tapering drugs.
Relapse : Worsening of rheumatic fever while under treatment and often with carditis.
Sub clinical carditis : When clinical examination is normal but echocardiogram is abnormal. Around 30 percent of patients having chorea present as sub clinical carditis.
Indolent carditis : It is a common entity in our country. Patient presents with persistent features of CHF, murmur and cardiomegaly. There are no or very few features of carditis.
Drugs For Control Of Inflammation In Acute Rheumatic Fever
| Inflammation |
Doses |
| Arthritis ± mild carditis Aspirin* |
Regime I
Starting doses: children 100 mg/kg/day for 2-3 weeks adult 6-8g/day - divide in 4-5 doses
Tapering doses :once symptoms resolved, taper to 60-70 mg/ kg/day.
For older children 50 mg/kg/day (Level of evidence : Class I)
Regime II
50 to 60 mg//kg /day for total 12 weeks (Level of evidence-Class Ib)
|
| Naproxen*(If aspirin intolerance detected) No response to aspirin in four days |
10-20 mg/kg/day Switch over to steroid. Rule out other conditions like chronic inflammatory/ myelo-proliferative disorders before switching over to steroids. |
| Moderate to severe carditis Steroids* |
Regime I
Prednisolone: 2mg/kg/d, maximum 80mg/day till ESR normalizes -usually 2 weeks.
Taper over 2-4 weeks, reduce dose by 2.5-5mg every 3rd day.
start aspirin 50-75mg/kg/d simultaneously, to complete total 12 weeks. (Level of evidence : Class I)
Regime II
Prednisolone same doses × 3-4 weeks. taper slowly to cover total period of 10-12 weeks (Level of evidence-Class IIb)
|
| Non responders Methyl Prednisolone (Intravenous) |
If no response to oral steroid therapy then start IV methyl prednisolone 30mg/kg/day for 3 days |
Management Of Atrial Fibrillation
Usually associated with chronic valvular heart disease.
Clinical presentation: irregularly irregular pulse.
ECG : Fibrillatory wave.
| Rate control |
(hemodynamically stable, untreated patients of rheumatic heart disease having chronic AF with fast AV conduction ) Digoxin*, Ca++ channel blocker*, beta blockers (Evidence level: Class I) |
| Rhythm control |
(hemodynamically unstable patients of chronic RHD having AF of recent onset),
Cardioversion** (level of evidence: Class I ),
Amiodarone infusion (Level of evidence: IIa)
|
| Anticoagulant |
Warfarin to achieve INR of 2-3 ( level of evidence: Class I)
Avoid vitamin K containing food like green leafy vegetables
|
Duration of secondary prophylaxis
- No carditis: 5 years/18yrs of age, whichever is longer.
- Mild to moderate carditis and healed carditis: 10 yrs/25 yrs of age, whichever is longer.
- Severe disease or post intervention patients: Life long.
One may opt for secondary prophylaxis up to the age of 40 years